Welcome to this comprehensive guide where we delve into the intriguing world of bronchitis and its impact on respiratory health. Bronchitis, a common respiratory condition characterized by the inflammation of the bronchial tubes, plays a significant role in our wellness narrative. Diving into the depths of this ailment, we encounter two prominent players: acute bronchitis, often triggered by viral infections, and chronic bronchitis, frequently linked to long-term exposure to irritants like smoking. Complicating the scene further, bacterial infections may also take center stage, intensifying symptoms and potential complications. And for those seeking an extended plotline, chronic bronchitis can become a part of the larger storyline known as chronic obstructive pulmonary disease (COPD). In this comprehensive exposition, we aim to explore the underlying causes, symptoms, and distinctions between acute bronchitis and chronic bronchitis. Additionally, we will spotlight conventional treatments while introducing an alternative approach that may prove beneficial—massage therapy. Our quest for knowledge will not end there; we shall equip you with essential precautions, lifestyle changes, and preventative measures to safeguard respiratory well-being. Embark with us on this journey as we uncover the secrets of effective bronchitis treatments and the therapeutic advantages of massage therapy.
Bronchitis, a common respiratory condition characterized by the inflammation of the bronchial tubes, plays a significant role in our wellness narrative. Diving into the depths of this ailment, we encounter two prominent players: acute bronchitis, often triggered by viral infections, and chronic bronchitis, frequently linked to long-term exposure to irritants like smoking. Complicating the scene further, bacterial infections may also take center stage, intensifying symptoms and potential complications. And for those seeking an extended plotline, chronic bronchitis can become a part of the larger storyline known as chronic obstructive pulmonary disease (COPD). In this comprehensive exposition, we aim to explore the underlying causes, symptoms, and distinctions between acute bronchitis and chronic bronchitis. Additionally, we will spotlight conventional treatments while introducing an alternative approach that may prove beneficial—massage therapy. Our quest for knowledge will not end there; we shall equip you with essential precautions, lifestyle changes, and preventative measures to safeguard respiratory well-being. Embark with us on this journey as we uncover the secrets of effective bronchitis treatments and the therapeutic advantages of massage therapy.
Bronchitis Causes
1. Chest Congestion: One of the primary causes of bronchitis is the inflammation of the bronchial tubes, leading to the accumulation of mucus in the chest. This congestion can result from viral or bacterial infections, triggering acute bronchitis. In chronic cases, irritants can cause long-term inflammation and persistent chest congestion.
2. Lung Irritants: Exposure to various irritants can irritate the bronchial tubes, leading to bronchitis. Common lung irritants include cigarette smoke, air pollution, chemical fumes, and dust. Prolonged exposure to these substances can significantly increase the risk of developing bronchitis.
Bronchitis Symptoms
1. Persistent Cough: The main symptom of bronchitis is a cough that may produce thickened mucus. The cough lasts for a few weeks, especially in chronic cases.
2. Shortness of Breath: As the bronchial tubes become inflamed and narrowed, it becomes challenging for air to pass through, resulting in shortness of breath.
3. Fatigue: Bronchitis can cause fatigue and weakness due to the body’s increased effort to combat the bacterial infection, and expel mucus.
4. Chest Discomfort: Individuals with bronchitis may experience chest discomfort or a feeling of tightness, often due to the accumulated mucus and inflammation in the airways.
5. Other Symptoms: Apart from the typical symptoms of acute bronchitis mentioned above, bronchitis can manifest with other signs such as mild fever, sore throat, and body aches.
Factors Making Symptoms Worse
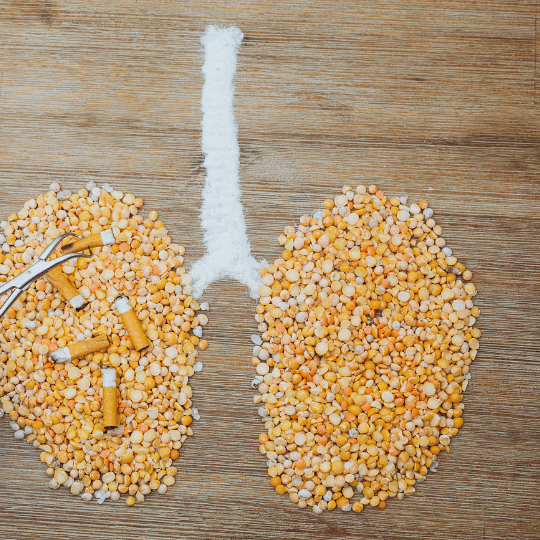 1. Smoking: Tobacco smoke is a major aggravating factor for bronchitis. It not only weakens the immune system but also introduces harmful chemicals into the respiratory system, intensifying inflammation and congestion.
1. Smoking: Tobacco smoke is a major aggravating factor for bronchitis. It not only weakens the immune system but also introduces harmful chemicals into the respiratory system, intensifying inflammation and congestion.
2. Allergens: For individuals with allergic bronchitis, exposure to allergens such as pollen, pet dander, or mold can exacerbate their symptoms.
3. Environmental Conditions: Cold and dry air can irritate the airways and worsen bronchitis. Indoor heating during winter months can also dry out the air and aggravate the underlying condition.
4. Weakened Immune System: A weakened immune system can make individuals more susceptible to bronchitis and may also delay the healing process.
Understanding the causes and symptoms of bronchitis is essential for prompt diagnosis and effective management. Congestion, lung irritants, and various other symptoms play a significant role in identifying and treating this respiratory condition. By recognizing these factors, individuals can take proactive steps to prevent bronchitis or seek appropriate medical attention for a speedy recovery.
Complications of Chronic Bronchitis
Chronic bronchitis, a long-term inflammation of the bronchial tubes, can lead to several complications if left untreated or poorly managed. Prolonged exposure to irritants and recurrent infections can cause damage to the airways, leading to COPD, a progressive and irreversible lung condition. Additionally, chronic bronchitis can weaken the respiratory system, making individuals more susceptible to severe respiratory infections like pneumonia. The persistent inflammation and excessive mucus production in the airways may result in respiratory difficulties, decreased lung function, and reduced physical activity tolerance. Over time, the strain on the heart from impaired lung function can contribute to heart problems, including cor pulmonale, a condition where the right side of the heart enlarges and weakens. Timely intervention, proper management, and lifestyle changes are essential to minimize the risk of complications associated with chronic bronchitis.
How to Diagnose Bronchitis
Diagnosing bronchitis typically involves a combination of medical history, physical examination, and sometimes additional tests. When a patient presents with symptoms like a cough, mucus production, and trouble breathing, the doctor will inquire about the duration and severity of symptoms, any exposure to irritants, smoking history, and previous respiratory conditions. During the physical exam, the doctor will listen to the patient’s lungs using a stethoscope to check for abnormal sounds like wheezing or crackles. While these steps can provide valuable clues, additional tests may be necessary for a conclusive diagnosis. These tests may include:
1. Chest X-ray: A chest X-ray can help rule out other respiratory conditions and identify any signs of lung inflammation or infection.
2. Pulmonary Function Test: These tests assess lung function and can help determine the presence and severity of airway obstruction, which is common in bronchitis.
3. Sputum Culture: Collecting a sample of mucus (sputum) and analyzing it for bacteria, viruses, or other pathogens can help identify the cause of bronchitis.
4. Blood Tests: Blood tests may be conducted to check for signs of infection or assess the patient’s overall health.
Diagnosing acute bronchitis is usually based on the patient’s symptoms and physical exam, while chronic bronchitis may require a more comprehensive evaluation to distinguish it from other chronic lung conditions. Once diagnosed, appropriate treatment and management strategies can be initiated to alleviate symptoms and prevent complications.
How To Prevent Acute Bronchitis
Preventing bronchitis involves adopting healthy habits and minimizing exposure to potential irritants and infections. Here are some effective ways to reduce the risk of developing bronchitis:
1. Avoid Smoking and Secondhand Smoke: If you smoke, quitting is the best step you can take to protect your respiratory health. Additionally, avoid exposure to secondhand smoke, as it can also lead to bronchitis and other respiratory problems.
2. Maintain Good Respiratory Hygiene: Cover your mouth and nose with a tissue or your elbow when coughing or sneezing to prevent the spread of respiratory infections. Dispose of used tissues properly and wash your hands regularly to reduce the risk of infections.
3. Limit Exposure to Air Pollutants: Minimize exposure to environmental irritants such as air pollution, chemical fumes, dust, and allergens. Use air purifiers in your home, and avoid outdoor activities during times of high pollution or allergen levels.
4. Stay Up-to-Date with Vaccinations: Make sure you and your family members receive recommended vaccinations, especially for influenza and pneumonia, as these infections can lead to bronchitis or worsen its symptoms.
5. Practice Good Hand Hygiene: Regularly wash your hands with soap and water, especially after being in public places or touching surfaces that may harbor germs.
6. Stay Hydrated: Drinking plenty of fluids helps keep the mucus in your airways moist and easier to expel, reducing the two risk factors of infection and congestion.
 7. Adopt a Healthy Lifestyle: Eat a balanced diet rich in fruits and vegetables to boost your immune system. Regular exercise can also enhance lung function and overall respiratory health.
7. Adopt a Healthy Lifestyle: Eat a balanced diet rich in fruits and vegetables to boost your immune system. Regular exercise can also enhance lung function and overall respiratory health.
8. Avoid Cold and Damp Environments: Dress appropriately for the weather and use a scarf or mask to cover your nose and mouth in the cold air, or damp conditions, as these factors can irritate the airways.
9. Seek Prompt Treatment for Respiratory Infections: If you develop symptoms of a respiratory infection, such as a cold or flu, seek medical attention promptly to prevent the infection from worsening and potentially leading to bronchitis.
10. Manage Chronic Health Conditions: If you have a chronic respiratory condition like asthma or COPD, work closely with your healthcare provider to manage it effectively and minimize the risk of bronchitis flare-ups.
By taking these preventive measures, you can significantly reduce the likelihood of developing bronchitis and maintain better respiratory health overall. If you have concerns about your respiratory health or experience persistent symptoms, consult a healthcare professional for personalized advice and care.
Conventional Bronchitis Treatments: Medications and Therapies
Conventional bronchitis treatments aim to relieve symptoms, reduce inflammation, and manage complications. The following are some common medications and therapies used in the treatment of bronchitis:
1. Bronchodilators: Bronchodilators are medications that help relax the muscles around the airways, widening them and making it easier to breathe. They are commonly used to treat bronchitis associated with conditions like asthma and COPD. Bronchodilators are available in various forms, including inhalers and nebulizers.
to breathe. They are commonly used to treat bronchitis associated with conditions like asthma and COPD. Bronchodilators are available in various forms, including inhalers and nebulizers.
2. Expectorants: Expectorants are over the counter medicines that help thin and loosen mucus, making it easier to cough up and expel from the lungs and airways. This can help relieve congestion and ease breathing. Guaifenesin is a commonly used expectorant that will help relieve the common cold and cough.
3. Cough Suppressants: Cough suppressants are used to reduce the frequency and intensity of a nagging cough. They are helpful for managing dry, non-productive coughs that do not produce mucus. However, they are not recommended for productive coughs that help clear mucus.
4. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen or naproxen, can help lessen inflammation and provide relief from pain and fever associated with acute bronchitis.
5. Antibiotics (in specific cases): Acute bronchitis is primarily caused by viruses, so taking antibiotics are generally not recommended unless a bacterial infection is suspected or confirmed. Overuse of antibiotics for lung infections can lead to antibiotic resistance, so they should only be prescribed when necessary.
6. Oxygen Therapy: In severe cases of bronchitis or when oxygen levels are low, oxygen therapy may be required. This involves providing supplemental oxygen through a mask or nasal cannula to ensure adequate oxygen levels in the blood.
7. Pulmonary Rehabilitation: For individuals with chronic bronchitis or underlying lung conditions, pulmonary rehabilitation programs can be beneficial. These programs include exercise training, education, and support to improve lung function and overall quality of life.
8. Hydration: Staying well-hydrated is essential for thinning mucus and promoting its expulsion from the airways. Drinking plenty of fluids can help ease congestion and soothe irritated airways.
9. Rest: Get plenty of rest. Adequate rest allows the body to focus on healing and fighting off infections, promoting a faster recovery from bronchitis.
10. Smoking Cessation: If the patient is a smoker, quitting smoking is crucial to prevent further damage to the airways and reduce the risk of recurrent bronchitis episodes.
It is important to note that these treatments are primarily used for managing symptoms and supporting the body’s natural healing process. In some cases, bronchitis can lead to complications or become chronic, requiring ongoing management and medical supervision.
How Massage Helps Alleviate Bronchitis Symptoms
Massage therapy can provide several benefits that may help individuals with bronchitis manage their symptoms and improve their overall well-being. While massage therapy cannot cure, it can complement conventional bronchitis treatments and promote relaxation and comfort. [Add Eucalyptus to your massage for more bang] Here are some ways in which massage therapy could be beneficial for individuals with bronchitis:
1. Relaxation and Stress Reduction: Massage therapy promotes relaxation and reduces stress, which can be beneficial for bronchitis patients. Stress can weaken the immune system and exacerbate bronchitis symptoms. By reducing stress levels, massage therapy may help support the body’s ability to fight infections and promote healing.
2. Improved Circulation: Massage can enhance blood circulation, which can aid in delivering more oxygen and nutrients to body tissues, including the lungs. Improved circulation may help alleviate congestion and reduce inflammation in the airways.
including the lungs. Improved circulation may help alleviate congestion and reduce inflammation in the airways.
3. Enhanced Respiratory Function: Certain massage techniques, such as chest and back percussion massage, can help loosen and mobilize mucus in the airways, making it easier than cough medicine alone to expel through coughing. This can provide relief from congestion and breathing difficulties.
4. Lymphatic Drainage: Massage therapy that includes lymphatic drainage techniques can assist in reducing swelling and promoting the removal of toxins and waste products from the body. This can aid the immune system in fighting respiratory infections.
5. Pain Relief: Massage therapy can help alleviate muscle tension and soreness often experienced by individuals with bronchitis due to coughing. By reducing pain and discomfort, massage can improve the overall quality of life during the illness.
6. Immune System Support: Some studies suggest that massage therapy can enhance the activity of natural killer cells, a type of immune cell responsible for fighting infections. This immune system support may aid in the body’s defense against bronchitis-causing pathogens.
It is essential to note that while massage therapy can offer these potential benefits, it should not be considered a substitute for medical treatment. Individuals with bronchitis should always follow their healthcare provider’s recommendations and take prescribed medications as advised. Before seeking massage therapy, it is crucial to consult with a qualified and experienced massage therapist to ensure that the chosen techniques are appropriate and safe for the individual’s specific condition.
In conclusion, incorporating massage therapy into your bronchitis management plan can offer numerous benefits, promoting relaxation, improving respiratory function, and providing relief from discomfort. If you’re seeking a professional and experienced massage center, look no further than Body Ache Escape Massage Center. Take a step towards enhancing your well-being and schedule a massage session now by clicking the “Schedule Now” button or calling us at 614-604-6358. Our skilled therapists are dedicated to providing personalized care to help you find comfort and relief on your journey to better respiratory health. Don’t wait; take charge of your well-being today!



