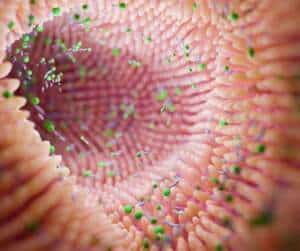
Depression is a mental health disorder that affects millions of people worldwide and can have dire consequences if left untreated. But what causes depression? It turns out, the answer may lie in your gut bacteria. Recent studies suggest that an imbalance in our gut microbiome could be at least partially responsible for triggering symptoms associated with depression.
left untreated. But what causes depression? It turns out, the answer may lie in your gut bacteria. Recent studies suggest that an imbalance in our gut microbiome could be at least partially responsible for triggering symptoms associated with depression.
In this article, we will discuss how imbalances in the gut’s microbiome are thought to contribute to feeling depressed. We’ll look at some of the scientific research surrounding this topic and explain why it is so important to maintain a healthy balance of beneficial bacteria within the digestive system. Finally, we’ll examine potential treatments and lifestyle modifications that can help restore microbial equilibrium and potentially reduce symptoms of depression.
Whether you’re currently dealing with depression or just want to know more about its possible causes, this article has something for everyone. Read on to learn how gut microbiota may cause – and possibly even prevent – depression!
Understanding The Link Between Gut Bacteria And Depression
The connection between gut bacteria and depression is an important topic of study. As the role of the microbiome in mental health continues to be explored, researchers are discovering that certain bacteria may play a significant part in treating depression. It’s not just any kind of bacteria; rather, it’s the composition of the microbiome as a whole that could have an impact on depression symptoms.
Gut microbes produce short chain fatty acids (SCFAs), which can affect brain chemistry by traveling through the vagus nerve. Some studies suggest that people with depression have different levels of SCFAs compared to those without it, suggesting that changes in our microbiomes could influence mood disorders like depression.
In addition to researching how various types of microbes might contribute to or improve depressive symptoms, scientists are also looking at ways to modify existing microbial populations within the gut so they can potentially reduce or eliminate symptoms that contribute to depression.
Exploring The Role Of Probiotics For Gut Bacteria
 Probiotics are live microorganisms that can help improve the good gut bacteria, and thus offer the potential for treating Major Depressive Disorder (MDD). For example, one study found that taking probiotics was able to reduce symptoms of depression by targeting specific areas of imbalance within the gut microbiome. Such studies suggest that manipulating the gut microbiome through supplementation could be used to alleviate some of the symptoms linked to depression.
Probiotics are live microorganisms that can help improve the good gut bacteria, and thus offer the potential for treating Major Depressive Disorder (MDD). For example, one study found that taking probiotics was able to reduce symptoms of depression by targeting specific areas of imbalance within the gut microbiome. Such studies suggest that manipulating the gut microbiome through supplementation could be used to alleviate some of the symptoms linked to depression.
These findings open up exciting possibilities when it comes to understanding and managing this common mental health condition. It is clear that there is still much more work needed before any definitive conclusions can be made about using probiotics as a treatment for depression, but a further exploration into this topic could yield promising results for those affected by it.
The best probiotics for balancing the gut microbiome depend on an individual’s specific needs. Some of the most popular include Lactobacillus acidophilus, Bifidobacterium, Saccharomyces boulardii, and Streptococcus thermophilus. Probiotics can be found in supplement form, or they can be obtained naturally through fermented foods such as yogurt, sauerkraut, kimchi, and kefir.
Importance of Gut Microbiome Diversity
The connection between the diversity of gut bacteria and emotional disorders is clear: people with lower levels of bacterial diversity in their guts are more likely to experience symptoms associated with depression and anxiety.

In addition to this, studies suggest that certain types of bacteria in the gut produce neurotransmitters like dopamine and serotonin which could improve mood or increase feelings of contentment.
As a result, we’re now seeing fecal microbiota transplantation (FMT) being used as a treatment for some cases of depression and anxiety. Fecal transplants involve transferring healthy microbes from one person’s gut into another person’s body via implanting fecal samples; this helps promote microbial diversity in the recipient’s digestive tract, potentially alleviating depressive symptoms by improving overall gut health.
Investigating The Role Of Serotonin In Depression
Serotonin is a neurotransmitter that affects brain function and mental well-being. It helps regulate mood, sleep, and appetite. Its presence in the body can be affected by various lifestyle factors, such as diet and medication use, but also by gut bacteria.
There is a complex relationship between serotonin and gut bacteria. Serotonin is produced in the digestive tract and is largely regulated by the bacteria that live in the gut. Certain types of gut bacteria can produce serotonin, while others can increase or decrease its production. Additionally, levels of serotonin may influence the types of bacteria that inhabit the gut, and vice versa.
This suggests the potential importance of a healthy gut and brain axis when it comes to managing depressive symptoms – both through maintaining an optimal level of beneficial bacteria in the gut, as well as using other strategies such as lifestyle modifications and medications where appropriate.
Foods high in the amino acid tryptophan can increase serotonin levels in the brain. These include salmon, eggs, spinach, nuts, seeds, and legumes. Also, taking supplements such as 5-HTP or St. John’s wort can help increase levels. Research shows that massage can increase serotonin levels in the brain by up to 28 percent. Massage can help increase levels by decreasing stress and releasing a hormone called oxytocin. Oxytocin helps reduce cortisol, the stress hormone. Massage can also help improve mood, reduce anxiety, and improve sleep quality. These all contribute to higher serotonin levels in the body.
Investigating The Role Of The Nervous System In Depression
 Recent studies suggest that there is more to the impact of the gut than just what meets the eye. The enteric nervous system (ENS) plays an important role in regulating mood-related hormones such as serotonin, which are associated with depressive symptoms. Moreover, changes in gut microbiota composition can alter ENS function and thereby affect both cognitive and emotional states.
Recent studies suggest that there is more to the impact of the gut than just what meets the eye. The enteric nervous system (ENS) plays an important role in regulating mood-related hormones such as serotonin, which are associated with depressive symptoms. Moreover, changes in gut microbiota composition can alter ENS function and thereby affect both cognitive and emotional states.
The ENS controls and coordinates the digestive system and is comprised of two main types of neurons: enteric sensory and motor neurons. Enteric sensory neurons detect changes in the environment, while motor neurons regulate muscle movement. Both types of neurons can produce serotonin, which is important for regulating intestinal function. This neurotransmitter helps to control appetite, digestion, and absorption of nutrients, as well as modulate the sensation of pain and inflammation.
Therefore, understanding how our central nervous system interacts with these elements within us could potentially lead to new treatments for depression by helping alleviate its symptoms through the manipulation of the body’s natural processes. Research into this area continues to grow, offering hope to many who struggle with this disorder every day.
Exploring The Role Of Butyrate In Depression
Butyrate is a short-chain fatty acid (SCFA) that is produced when bacteria in the gut break down dietary fiber. It is an important energy source for the cells lining the colon and has been linked to many health benefits, including improved digestion and increased protection against colon cancer.
This fatty acid acts as an anti-inflammatory agent and helps to promote a healthy balance of gut bacteria. It also helps to protect the lining of the gut, reducing the risk of leaky gut syndrome. Additionally, it can help to reduce the risk of certain types of cancer, improve digestion, and support the immune system.
Fecal microbiota transplantation (FMT) is one way researchers believe they can improve your levels of this important fatty acid. Some other ways to improve your levels of butyrate are: exercise, increasing your dietary fiber intake, taking a prebiotic and probiotic, and eating probiotic foods like yogurt.
Investigating The Role Of The Vagus Nerve In Depression
The vagus nerve is a major component of the human body’s nervous system, and its role in depression has been increasingly studied. It connects the brain to many organs throughout the body, including those involved in controlling digestion and other processes related to gut health.
increasingly studied. It connects the brain to many organs throughout the body, including those involved in controlling digestion and other processes related to gut health.
This nerve helps to regulate the gut microbiome composition. The nerve can signal the body to increase or decrease the production of certain hormones that affect the growth of bacteria. It can also influence the activity of immune cells that help protect the body from harmful bacteria. Additionally, the vagus nerve helps coordinate the movement of food and liquid through the digestive tract, which helps to maintain the balance of bacteria in the gut.
The vagus nerve is involved in controlling the body’s fight-or-flight response, and it has been linked to mood regulation. Stimulating the nerve can help to reduce symptoms of depression by decreasing cortisol levels and increasing serotonin levels. This can help to reduce stress and anxiety as well as improve mood. Stimulation of the vagus nerve can be done through a variety of techniques such as deep breathing, yoga, and meditation.
Examining The Impact Of Medication Use On Gut Bacteria
Medication use may play a role in depression. Medications used to change the balance and population of bacteria in the body may also impact symptoms of depression.
For example, studies have indicated that antibiotics can reduce levels of certain types of gut bacteria that are linked to depressive behaviors. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, steroids, proton pump inhibitors (PPIs), and antacids can all be harmful to gut bacteria.
If further research indicates there is a link between certain medications and improved outcomes related to depression, then this could offer new avenues for therapeutic treatment or prevention strategies among those who suffer from it.
Conclusion
In conclusion, the link between our gut microbiome and depression is real. Research has shown that probiotics can play a role in helping manage symptoms of depression. The gut microbiome has an impact on brain chemistry, as well as serotonin levels. Additionally, there may be a relationship between the nervous system and depression due to changes in fecal microbiota.
It’s clear that improving one’s gut health is important when managing depression. This means being mindful of lifestyle factors such as exercise, diet, and sleep habits can all have an effect on mental well-being. Finally, medication use should always be discussed with your doctor before taking any action – medications are not necessarily a cure for depression but could provide relief from symptoms if used correctly.
Massage can help improve gut health in several ways. It can reduce stress and anxiety, which can impact digestive health. Massage can also help reduce inflammation, improve circulation, and promote relaxation. This can all aid in the body’s ability to absorb nutrients more effectively and improve digestion. Massage helps to break down and move food that is stuck in the digestive tract, helping to prevent constipation and other digestive issues. Schedule here.
At the end of the day, understanding how our gut affects our emotional state is essential for anyone who wants to seek out better mental health outcomes. With further research into this area, we will gain more insight into how we can best take care of ourselves both mentally and physically.