Everyone understands how fitness benefits your body. But its benefits for your mind are gaining mainstream attention: more and more research indicates exercise protects against chronic stress, depression, anxiety, and other mental health conditions.
Heart disease remains a leading cause of death globally, yet its relationship with mental health, particularly depression, often goes unnoticed. Research, including insights from Johns Hopkins Medicine, reveals a complex interaction where depression not only arises as a result of heart disease but can also precede and exacerbate it. This dual threat underscores the critical need for integrated care approaches addressing heart health and mental well-being to improve overall patient outcomes. Understanding this connection is vital for effective prevention and treatment strategies.
How Depression and Heart Disease Relate to Each Other
Understanding the Link
The relationship between depression and heart disease is bidirectional, posing a complex challenge in the medical and mental health fields. Depression can significantly increase the risk of developing heart disease, as it affects the body’s cardiovascular system by altering heart rate and blood pressure and influencing hormonal balance.
Conversely, experiencing heart disease can lead to depression, often due to the emotional and physical strain of dealing with a serious illness. This cyclical link necessitates a comprehensive treatment and prevention approach that addresses psychological and physiological aspects to improve overall health outcomes.
The Signs of Depression
Depression manifests in various forms, and when related to heart disease, certain symptoms are particularly prevalent. Individuals with heart disease may experience a range of emotional and psychological signs that signal depression:
- Persistent sadness or low mood
- Loss of interest in activities once enjoyed
- Fatigue and decreased energy
- Difficulty sleeping or oversleeping
- Changes in appetite and weight
- Feelings of hopelessness or helplessness
- Unexplained physical symptoms, such as headaches or muscle pain
- Difficulty concentrating, remembering, or making decisions
- Increased irritability or frustration, even over small matters
Recognizing these symptoms is crucial for early intervention and management, potentially mitigating the severity of both heart disease and depression.
Higher Rates of Heart Disease Among People with Depression
Impact of Mental Health on Cardiovascular Health
Mental health, particularly depression, has a significant impact on cardiovascular health, influencing both the incidence and progression of heart disease. Depression can lead to several physiological changes that increase the risk for heart disease:
- Increased Inflammatory Response: Depression is associated with heightened inflammation, a critical factor in coronary artery disease.
- Altered Autonomic Nervous System: Depression can affect the autonomic nervous system, which controls heart rate and blood pressure, potentially leading to arrhythmias and hypertension.
- Behavioral Factors: Individuals with depression may exhibit behaviors that compromise heart health, including poor diet, physical inactivity, and non-compliance with medical regimens.
- Endothelial Dysfunction: Depression has been linked to dysfunction of the endothelium, the inner lining of blood vessels, which can reduce blood flow and increase the risk of atherosclerotic buildup.
Recognizing and treating depression early in patients at risk for or living with heart disease is crucial for preventing cardiovascular events and improving overall health outcomes.
Treating Depression to Improve Heart Health
Effectively treating depression not only aids in mental health recovery but also reduces the risk of heart disease. Here are key treatment options that can benefit both depression and heart health:
- Antidepressant Medication: Certain antidepressants have been shown to improve mood without negatively impacting heart health.
- Psychotherapy: Techniques such as cognitive-behavioral therapy (CBT) help manage stress and negative thoughts, reducing mental strain and improving cardiovascular health.
- Lifestyle Modifications: Encouraging regular physical activity, a balanced diet, and sufficient sleep can greatly improve both depression and heart health.
- Cardiac Rehabilitation and Support Groups: Participating in cardiac rehabilitation that includes psychological support can help patients manage both heart disease and depression more effectively.
Integrating these treatments can create a comprehensive approach that supports overall health, addressing the intricate connection between mental and cardiovascular health.

Exercise, the Simplest Prevention Tool
Regular exercise is a powerful strategy for combating both depression and heart disease, proving to be one of the most effective preventive measures. Engaging in physical activity boosts cardiovascular health by improving blood flow, reducing blood pressure, and enhancing overall heart function. Simultaneously, exercise acts as a natural antidepressant, stimulating the release of endorphins that elevate mood and reduce stress. [How Much Exercise Prevents Depression]
For those at risk of or managing heart disease and depression, incorporating a routine of moderate exercise can significantly enhance quality of life and reduce the incidence of these conditions. Integrating this simple yet effective tool into daily life supports long-term health and well-being, demonstrating its role as a foundational element in managing both mental and physical health.
Recent research highlights that maintaining high fitness levels in mid-life, particularly in one’s forties and fifties, is associated with a reduced risk of developing depression after the age of 65, as well as a decreased risk of mortality from heart disease, regardless of depression status.
Dr. Benjamin Willis, the study’s lead author and director of epidemiology at The Cooper Institute, emphasizes the significant long-term advantages of physical fitness for both mental and physical health.
The findings from a study spanning four decades with nearly 18,000 U.S. adults demonstrate a clear correlation between sustained physical activity and improved cardiovascular and mental health outcomes. The study, published in JAMA Psychology, underscores aerobic exercise as a key strategy for enhancing fitness and preventing heart disease. [Exercise Now, Avoid Depression Later]
Self-Care For Those With Depression Symptoms
Embracing regular physical activity and maintaining mental health is crucial in mitigating the risks associated with cardiovascular disease and heart failure. The American Heart Association highlights that exercise and psychological well-being are significant preventative measures against heart disease. Individuals experiencing depression are at a higher risk of cardiac events, emphasizing the importance of managing mental health as a critical risk factor. By addressing both physical and mental health, we can effectively lower the risk of heart disease and improve overall health outcomes.
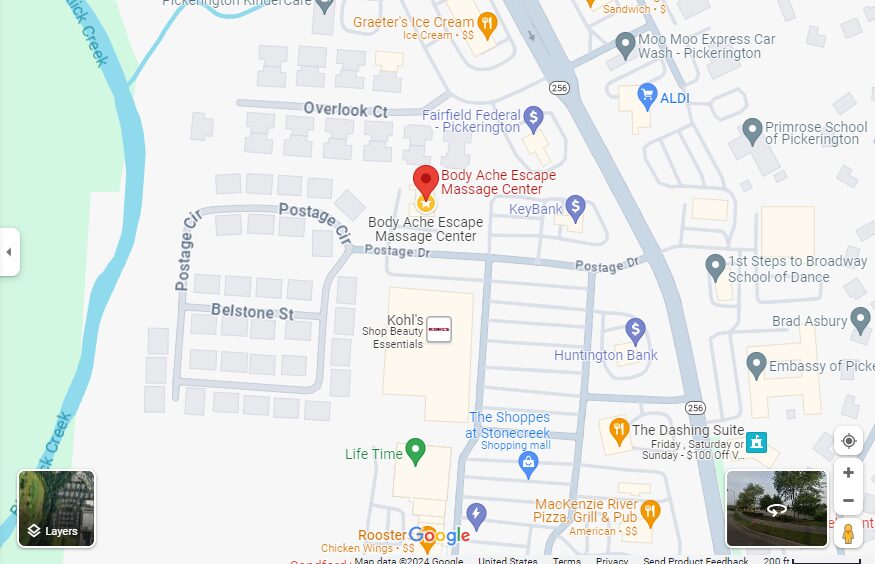
To further support your journey towards better heart and mental health, consider booking a massage at Body Ache Escape. A professional massage can reduce stress, improve circulation, and enhance overall well-being, all contributing to a healthier heart and a happier mind. Take a proactive step towards your health today and allow us to help you achieve a more balanced lifestyle. Visit us at Body Ache Escape to schedule your session and start feeling better inside and out. [Massage and Depression]